What is Keratoconus?
Keratoconus is a progressive eye condition that affects the structure and shape of the cornea. The cornea, is made of multiple layers which can gradually thin and bulge into a cone-like shape, leading to distorted and blurry vision. The cornea is the clear domed front surface of the eye and is the main component affect when focusing (refracting) light within the eye. A healthy cornea is essential to achieving good vision
What causes Keratoconus?
Keratoconus is a progressive condition which usually starts during childhood or teenage years, with deterioration possible until around 40 years. It affects both eyes but can develop at different rates in each eye. While the exact cause of keratoconus is not fully understood, it is believed to involve a combination of genetic and environmental factors. Potential genetic markers have been identified, suggesting a familial predisposition to the condition. Additionally, the habitual rubbing of eyes, excessive exposure to ultraviolet (UV) light, and certain medical conditions such as asthma and allergies also appear to play a role. However, as we age the progression of keratoconus typically slows and eventually halts.
How is Keratoconus diagnosed?
To ascertain the presence of keratoconus, an eye care professional at Vision Care Clinic will perform a comprehensive eye examination. This involves a thorough clinical examination, a review of your ophthalmic history and detailed corneal scanning including techniques such as corneal topography, tomography and aberrometry. These assessments aid in accurate diagnosis and help determine the appropriate treatment plan.
How is Keratoconus treated?
While a diagnosis of keratoconus may seem daunting, there are effective treatment options available to both stabilise the shape of the cornea and also to regularise the cornea and improve vision . At Vision Care Clinic, our specialists offer an extensive range of treatments for keratoconus, depending on the severity, progression and desired outcome. We understand the challenge of this eye condition is unique to each individual patient, which is why we utilise the latest technology to offer an accurate diagnosis to confirm the stage and extent of the corneal disease. Also, enabling us to recommend an informed, bespoke treatment plan for optimal results based on accurate data.
Uniquely, Vision Care Clinic can offer patients with keratoconus the opportunity to stabilise the shape of their cornea and even regenerate their vision with one, or a combination of treatments available at our practice. While many keratoconus treatments simply halt the progression of the disease, our award-winning doctors offer the opportunity of visual rehabilitation, resulting in improved corrected vision and potentially less dependence on glasses.
FAQ
Who is at risk of keratoconus?
Keratoconus affects 55 in 100,000. It is linked to genetics and conditions such as allergic eye disease and hayfever.
It is thought that repeated rubbing of the eyes can weaken the cornea.
What are the symptoms of keratoconus?
Symptoms depend on the stage of the disease and severity.
Patients may start by noticing increased light sensitivity and the need to change their glasses prescription more frequently. However, there can be a limit to the visual improvement achieved with glasses and contact lenses. Keratoconus can be progressive and, if left untreated, may result in poor quality of vision, corneal warpage and even the need for a corneal graft.
How is keratoconus stabilised?
Initially, we aim to stabilise the cornea and stop it from progressively changing shape due to its weakened structure.
For some patients, further procedures to improve the quality of their vision are available. These include laser eye surgery and inserting intrastromal corneal rings to reshape the cornea.
If keratoconus is advanced, some patients may still require a corneal graft.
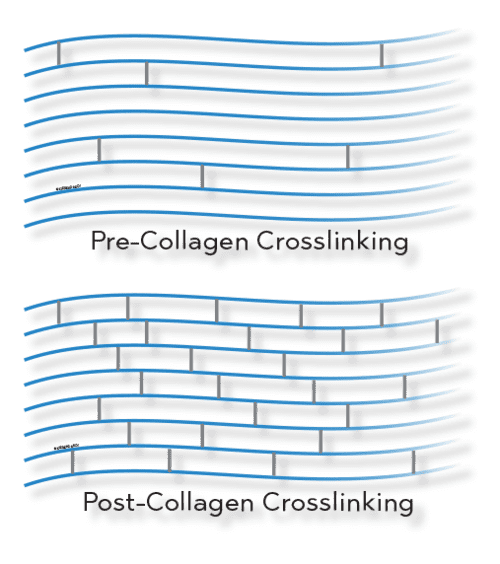
Corneal cross-linking:
Corneal cross-linking (CXL) is a procedure that strengthens the cornea to halt the progression of keratoconus. The number of corneal grafts now performed for keratoconus has dramatically fallen since the advent of CXL.
Cross-linking is an outpatient procedure performed with anaesthetic drops to numb the eye. The prepared cornea is soaked with special vitamin B drops, which are then activated using a specialist ultraviolet light to the eye. The procedure takes around 20 minutes per eye. A bandaged contact lens is applied at the end of the procedure. This acts like a transparent plaster while the eye heals. The lens is left in-situ until being removed in the clinic a few days later. It is essential to avoid any water contact with contact lenses.
Corneal graft:
A corneal graft is performed to replace diseased or scarred tissue with healthy donor tissue. These can be performed at different depths depending on the condition being treated and the layers of the cornea affected. Patients may need a corneal graft in severe and advanced stages of keratoconus. However, the need for corneal grafts has reduced since corneal cross-linking was introduced.
Can vision be improved?
The good news is that patients with keratoconus can also benefit from procedures to improve their vision. At Vision Care Clinic, we offer a wide range of advanced techniques, which are often used in combination and coupled with corneal crosslinking to stabilise the results for the long term.
Customised laser eye surgery:
For some patients, combined customised laser eye surgery and cross-linking is beneficial. Firstly, laser eye surgery is used to reshape the cornea and make it more regular, improving the quality of vision in glasses. Cross-linking is then used to stabilise and strengthen the corneal tissue. After the keratoconus has been stabilised, further procedures can often be performed to reduce an individual’s reliance on contact lenses or glasses.
Intra–stromal corneal rings:
Intra-corneal stromal rings are small, transparent rings inserted into tiny channels at precise depths with a laser within the cornea. These provide additional structural support to improve the shape of the cornea and the quality of vision. These rings can be made from biological tissue, closely matching the existing cornea (CAIRS – Corneal allogenic intrastromal ring segments) or plastic (Keraring, Intacs). After the rings have reshaped the cornea, this may be followed by other procedures, such as cross-linking or laser eye surgery.
Corneal graft:
A corneal graft is performed to replace diseased or scarred tissue with healthy donor tissue. These can be performed at different depths depending on the condition being treated and the layers of the cornea affected. Keratoconus typically affects the outer and middle layers of the cornea, and the need for corneal grafts has reduced since the introduction of corneal cross-linking. Examples of corneal transplants for keratoconus include DALK (deep anterior lamellar keratoplasty), PK (Penetrating keratoplasty), BLT (Bowmans layer transplant).
What should I do if I’ve been advised that I have keratoconus?
We recommend a full consultation with our corneal specialist. This will include a thorough clinical examination with the most advanced scans to ascertain progression and effect. After this, a potential treatment plan will be suggested and explained.

CAIRS Procedure
Corneal allogenic intrastromal ring segments or CAIRS is the latest treatment for keratoconus and is performed using donor corneal tissue, which is processed and prepared into either rings or arcs.
The treatment involves inserting either the selected ring or arc of corneal tissue into the recipient cornea, to achieve a flatter more regularised surface. This treatment option can delay and prevent the need for corneal graft surgery, improve vision and potentially, leads the way to laser eye surgery to further vision enhancement.
Our CAIRS procedure provides increased biocompatibility, compared to previously used plastic implants, resulting in comfortable eyes and no reported cases of increased halos or glare around lights at night. The procedure is performed in a clean room, using topical anaesthetic eye drops and is reversible.
Contact us today for a keratoconus consultation
Keratoconus may pose challenges to those affected, but with early detection and appropriate treatment, patients can regain visual clarity and enjoy an improved quality of life.
Vision Care Clinic offers a consultant-led relationship from the initial keratoconus consultation through to the bespoke treatment plan and after-care. If you’re concerned about the progression of your keratoconus and would like the opportunity to improve your visual quality, contact our team at Vision Care Clinic on 0117 905 7722 to book in for your consultation. Vision Care Clinic is based in Bristol and treats keratoconus patients from across the UK and further afield.